Duchenne muscular dystrophy
| Duchenne muscular dystrophy | |
|---|---|
 | |
| Microscopic image of cross-sectional calf muscle from a person with Duchenne muscular dystrophy, showing extensive replacement of muscle fibers by fat cells. | |
| Pronunciation | |
| Specialty | Pediatric neurology, neuromuscular medicine, medical genetics |
| Symptoms | Muscle weakness, trouble standing up, scoliosis[2][3][4] |
| Usual onset | Around age 4[2] |
| Causes | Genetic (X-linked recessive)[3] |
| Diagnostic method | Genetic testing[3] |
| Treatment | Pharmacological treatment, physical therapy, braces, speech therapy, occupational therapy, surgery, assisted ventilation[2][3] |
| Medication | Corticosteroids |
| Prognosis | life expectancy of 21–40 years[5] |
| Frequency | In males, 1 in 3,500-6,000[3] In females, 1 in 50,000,000[6] |
Duchenne muscular dystrophy (DMD) is a severe type of muscular dystrophy predominantly affecting boys.[3][7][8] The onset of muscle weakness typically begins around age four, with rapid progression.[2] Initially, muscle loss occurs in the thighs and pelvis, extending to the arms,[3] which can lead to difficulties in standing up.[3] By the age of 12, most individuals with Duchenne muscular dystrophy are unable to walk.[2] Affected muscles may appear larger due to an increase in fat content,[3] and scoliosis is common.[3] Some individuals may experience intellectual disability,[3] and females carrying a single copy of the mutated gene may show mild symptoms.[3]
Duchenne muscular dystrophy is caused by mutations or deletions in any of the 79 exons encoding the large dystrophin protein, which is essential for maintaining the muscle fibers' cell membrane integrity.[3] The disorder follows an X-linked recessive inheritance pattern, with approximately two-thirds of cases inherited from the mother and one-third resulting from a new mutation.[3] Diagnosis can frequently be made at birth through genetic testing, and elevated creatine kinase levels in the blood are indicative of the condition.[3]
While there is no known cure, management strategies such as physical therapy, braces, and corrective surgery may alleviate symptoms.[2] Assisted ventilation may be required in those with weakness of breathing muscles.[3] Several drugs designed to address the root cause are currently available including gene therapy (Elevidys), and antisense drugs (Ataluren, Eteplirsen etc.).[3] Other medications used include glucocorticoids (Deflazacort, Vamorolone); calcium channel blockers (Diltiazem); to slow skeletal and cardiac muscle degeneration, anticonvulsants to control seizures and some muscle activity, and Histone deacetylase inhibitors (Givinostat) to delay damage to dying muscle cells.[2][3]
Various figures of the occurrence of Duchenne muscular dystrophy are reported. One source reports that it affects about one in 3,500 to 6,000 males at birth.[3] Another source reports Duchenne muscular dystrophy being a rare disease and having an occurrence of 7.1 per 100,000 male births.[9] A number of sources referenced in this article indicate an occurrence of 6 per 100,000.[10]
Duchenne muscular dystrophy is the most common type of muscular dystrophy,[3] with a median life expectancy of 27–31 years.[5][11] However, with comprehensive care, some individuals may live into their 30s or 40s.[3] Duchenne muscular dystrophy is considerably rarer in females, occurring in approximately one in 50,000,000 live female births.[6]
Signs and symptoms
[edit]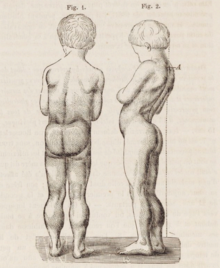
Duchenne muscular dystrophy causes progressive muscle weakness due to muscle fiber disarray, death, and replacement with connective tissue or fat.[3] The voluntary muscles are affected first, especially those of the hips, pelvic area, thighs, calves.[3][2][12] It eventually progresses to the shoulders and neck, followed by arms, respiratory muscles, and other areas.[12] Fatigue is common.[13]
Signs usually appear before age five, and may even be observed from the moment a boy takes his first steps.[14] There is general difficulty with motor skills, which can result in an awkward manner of walking, stepping, or running.[15] They tend to walk on their toes,[15] in part due to shortening of the Achilles tendon,[16] and because it compensates for knee extensor weakness.[12] Falls can be frequent.[17] It becomes increasingly difficult for the boy to walk. His ability to walk usually disintegrates completely before age 13.[15] Most men affected with Duchenne muscular dystrophy become essentially "paralyzed from the neck down" by the age of 21.[14] Cardiomyopathy, particularly dilated cardiomyopathy, is common, seen in half of 18-year-olds.[15] The development of congestive heart failure or arrhythmia (irregular heartbeat) is only occasional.[12] In late stages of the disease, respiratory impairment and swallowing impairment can occur, which can result in pneumonia.[18]

A classic sign of Duchenne muscular dystrophy is trouble getting up from lying or sitting position,[17] as manifested by a positive Gowers's sign. When a child tries to arise from lying on his stomach, he compensates for pelvic muscle weakness through use of the upper extremities:[15] first by rising to stand on his arms and knees, and then "walking" his hands up his legs to stand upright. Another characteristic sign of Duchenne muscular dystrophy is pseudohypertrophy (enlarging) of the muscles of the tongue, calves, buttocks, and shoulders (around age 4 or 5). The muscle tissue is eventually replaced by fat and connective tissue, hence the term pseudohypertrophy. Muscle fiber deformities and muscle contractures of Achilles tendon and hamstrings can occur, which impair functionality because the muscle fibers shorten and fibrose in connective tissue.[12] Skeletal deformities can occur, such as lumbar hyperlordosis, scoliosis, anterior pelvic tilt, and chest deformities. Lumbar hyperlordosis is thought to be compensatory mechanism in response to gluteal and quadriceps muscle weakness, all of which cause altered posture and gait (e.g.: restricted hip extension).[19][20]
Non musculoskeletal manifestations of Duchenne muscular dystrophy occur. There is a higher risk of neurobehavioral disorders (e.g., ADHD), learning disorders (dyslexia), and non-progressive weaknesses in specific cognitive skills (in particular short-term verbal memory),[15] which are believed to be the result of inadequate dystrophin in the brain.[21]
Cause
[edit]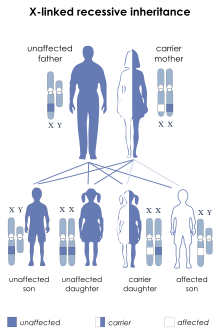
Duchenne muscular dystrophy is caused by a mutation of the dystrophin gene, located on the short arm of the X chromosome (locus Xp21)[22] that codes for dystrophin protein. Mutations can either be inherited or occur spontaneously during germline transmission,[citation needed] causing a large reduction or absence of dystrophin, a protein that provides structural integrity in muscle cells.[23] Dystrophin is responsible for connecting the actin cytoskeleton of each muscle fiber to the underlying basal lamina (extracellular matrix), through a protein complex containing many subunits. The absence of dystrophin permits excess calcium to penetrate the sarcolemma (the muscle cell membrane).[24]

Duchenne muscular dystrophy is extremely rare in females (about 1 in 50,000,000 female births).[6] It can occur in females with an affected father and a carrier mother, in those who are missing an X chromosome, or those who have an inactivated X chromosome (the most common of the rare reasons).[25] The daughter of a carrier mother and an affected father will be affected or a carrier with equal probability, as she will always inherit the affected X-chromosome from her father and has a 50% chance of also inheriting the affected X-chromosome from her mother.[26]
Disruption of the blood–brain barrier has been seen to be a noted feature in the development of Duchenne muscular dystrophy.[27]
Diagnosis
[edit]Duchenne muscular dystrophy can be detected with about 95% accuracy by genetic studies performed during pregnancy.[18]
DNA test
[edit]The muscle-specific isoform of the dystrophin gene is composed of 79 exons, and DNA testing (blood test) and analysis can usually identify the specific type of mutation of the exon or exons that are affected. DNA testing confirms the diagnosis in most cases.[28]
Muscle biopsy
[edit]If DNA testing fails to find the mutation, a muscle biopsy test may be performed.[29] A small sample of muscle tissue is extracted using a biopsy needle. The key tests performed on the biopsy sample for Duchenne muscular dystrophy are immunohistochemistry, immunocytochemistry, and immunoblotting for dystrophin, and should be interpreted by an experienced neuromuscular pathologist.[30] These tests provide information on the presence or absence of the protein. Absence of the protein is a positive test for Duchenne muscular dystrophy. Where dystrophin is present, the tests indicate the amount and molecular size of dystrophin, helping to distinguish Duchenne muscular dystrophy from milder dystrophinopathy phenotypes.[31] Over the past several years, DNA tests have been developed that detect more of the many mutations that cause the condition, and muscle biopsy is not required as often to confirm the presence of Duchenne muscular dystrophy.[32]
Prenatal tests
[edit]A prenatal test can be considered when the mother is a known or suspected carrier.[33]
Prior to invasive testing, determination of the fetal sex is important; while males are sometimes affected by this X-linked disease, female Duchenne muscular dystrophy is extremely rare. This can be achieved by ultrasound scan at 16 weeks or more recently by free fetal DNA (cffDNA) testing. Chorion villus sampling (CVS) can be done at 11–14 weeks, and has a 1% risk of miscarriage. Amniocentesis can be done after 15 weeks, and has a 0.5% risk of miscarriage. Non invasive prenatal testing can be done around 10–12 weeks.[34] Another option in the case of unclear genetic test results is fetal muscle biopsy.[citation needed]
Treatment
[edit]
No cure for Duchenne muscular dystrophy is known.[35]
Treatment is generally aimed at controlling symptoms to maximize the quality of life which can be measured using specific questionnaires,[36] and include:
- Corticosteroids such as prednisolone, deflazacort and Vamorolone (Agamree) lead to short-term improvements in muscle strength and function up to 2 years.[37] Corticosteroids have also been reported to help prolong walking, though the evidence for this is not robust.[38]
- Disease-specific physical therapy is helpful to maintain muscle strength, flexibility, and function. It aims to:[39]
- Minimize the development of contractures and deformity by developing a programme of stretches and exercises where appropriate
- Anticipate and minimize other secondary complications of a physical nature by recommending bracing and durable medical equipment[40]
- Monitor respiratory function and advise on techniques to assist with breathing exercises and methods of clearing secretions[39]
- Orthopedic appliances (such as braces and wheelchairs) may improve mobility and the ability for self-care. Form-fitting removable leg braces that hold the ankle in place during sleep can defer the onset of contractures.
- Appropriate respiratory support as the disease progresses is important.
- Cardiac problems may require a pacemaker.[41]
The medication eteplirsen, a Morpholino antisense oligo, has been approved in the United States for the treatment of mutations amenable to dystrophin exon 51 skipping. The US approval has been controversial[42] as eteplirsen failed to establish a clinical benefit;[43] it has been refused approval by the European Medicines Agency.[44][45]
The medication ataluren (Translarna) is approved for use in the European Union.[46][47]
The antisense oligonucleotide golodirsen (Vyondys 53) was approved for medical use in the United States in 2019, for the treatment of cases that can benefit from skipping exon 53 of the dystrophin transcript.[48][49]
The Morpholino antisense oligonucleotide viltolarsen (Viltepso) was approved for medical use in the United States in August 2020, for the treatment of Duchenne muscular dystrophy (DMD) in people who have a confirmed mutation of the DMD gene that is amenable to exon 53 skipping.[50] Developed by Nippon Shinyaku and the National Center of Neurology and Psychiatry (NCNP), viltolarsen's pre-clinical development was supported by pioneering work from Toshifumi Yokota and colleagues.[51] It is the second approved targeted treatment for people with this type of mutation in the United States.[50] Approximately 8% of people with DMD have a mutation that is amenable to exon 53 skipping.[50]
Casimersen (Amondys 45) was approved for medical use in the United States in February 2021,[52] and it is the first FDA-approved targeted treatment for people who have a confirmed mutation of the Duchenne muscular dystrophy gene that is amenable to exon 45 skipping.[52]
Comprehensive multidisciplinary care guidelines for Duchenne muscular dystrophy have been developed by the US Centers for Disease Control and Prevention, and were published in 2010.[29] An update was published in 2018.[53][54]
Delandistrogene moxeparvovec (Elevidys) is a gene therapy that in June 2023 received United States FDA accelerated approval for treatment of four and five-year-old children.[55][56]
In March 2024, the US Food and Drug Administration (FDA) granted approval for givinostat (Duvyzat), an oral medication, to be used in the treatment of Duchenne muscular dystrophy in people aged six years and older. Givinostat is the first nonsteroidal drug to receive FDA approval for the treatment of all genetic variants of Duchenne muscular dystrophy. Functioning as a histone deacetylase (Histone deacetylase (HDAC) inhibitor, givinostat operates by targeting pathogenic processes within the body, ultimately leading to a reduction in inflammation and muscle loss associated with the disease.[57]
Prognosis
[edit]Duchenne muscular dystrophy is a rare progressive disease which eventually affects all voluntary muscles and involves the heart and breathing muscles in later stages. Life expectancy is estimated to be around 25–26,[18][58] but this varies. People born with Duchenne muscular dystrophy after 1990 have a median life expectancy of approximately 28–30.[11][5] With excellent medical care, affected men often live into their 30s.[59] The oldest surviving person in the world with the disease is 60 years old.[60][61]
The most common direct cause of death in people with Duchenne muscular dystrophy is respiratory failure. Complications from treatment, such as mechanical ventilation and tracheotomy procedures, are also a concern. The next leading cause of death is cardiac-related conditions such as heart failure brought on by dilated cardiomyopathy. With respiratory assistance, the median survival age can reach up to 40. In rare cases, people with Duchenne muscular dystrophy have been seen to survive into their forties or early fifties, with proper positioning in wheelchairs and beds, and the use of ventilator support (via tracheostomy or mouthpiece), airway clearance, and heart medications.[62] Early planning of the required supports for later-life care has shown greater longevity for people with Duchenne muscular dystrophy.[63]
Curiously, in the mdx mouse model of Duchenne muscular dystrophy, the lack of dystrophin is associated with increased calcium levels and skeletal muscle myonecrosis. The intrinsic laryngeal muscles (ILMs) are protected and do not undergo myonecrosis.[64] ILMs have a calcium regulation system profile suggestive of a better ability to handle calcium changes in comparison to other muscles, and this may provide a mechanistic insight for their unique pathophysiological properties.[65] In addition, patients with Duchenne muscular dystrophy also have elevated plasma lipoprotein levels, implying a primary state of dyslipidemia in patients.[66]
Epidemiology
[edit]Duchenne muscular dystrophy is the most common type of muscular dystrophy; it affects about one in 5,000 males at birth.[3] Duchenne muscular dystrophy has an incidence of one in 3,600 male infants.[18]
In the US, a 2010 study showed a higher amount of those with Duchenne muscular dystrophy age ranging from 5 to 54 who are Hispanic compared to non-Hispanic Whites, and non-Hispanic Blacks.[67][68]
History
[edit]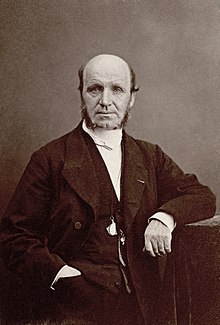
The disease was first described by the Neapolitan physician Giovanni Semmola in 1834 and Gaetano Conte in 1836.[69][70][71] However, Duchenne muscular dystrophy is named after the French neurologist Guillaume-Benjamin-Amand Duchenne (1806–1875), who in the 1861 edition of his book Paraplégie hypertrophique de l'enfance de cause cérébrale, described and detailed the case of a boy who had this condition. A year later, he presented photos of his patient in his Album de photographies pathologiques. In 1868, he gave an account of 13 other affected children. Duchenne was the first to do a biopsy to obtain tissue from a living patient for microscopic examination.[72][73]
Society and culture
[edit]Notable cases
[edit]- Alfredo Ferrari was an Italian automotive engineer, the eldest son of automaker Enzo Ferrari, and the planned heir to his father's sports car company, Ferrari. Alfredo died of DMD on 30 June 1956 at the age of 24.[74][75]
- Rapper and disability rights advocate Darius Weems had the disease and used his notoriety to raise awareness and funds for treatment, as seen in the documentary Darius Goes West (2007).[76] He died at the age of 27 in 2016.[77]
- Jonathan Evison's novel, The Revised Fundamentals of Caregiving, published in 2012, depicted a young man affected by the disease. In 2016, Netflix released The Fundamentals of Caring, a film based on the novel.[78]
- Mats Steen, also known by his in-game character name, Ibelin, was a Norwegian gamer affected by Duchenne who became widely known posthumously after his parents discovered the extensive online community he had formed through the game World of Warcraft. In 2024, Netflix released The Remarkable Life of Ibelin, a documentary depicting his life and the aftermath of his death.
Research
[edit]This section needs to be updated. (August 2019) |
Efforts are ongoing to find medications that either return the ability to make dystrophin or utrophin.[79] Other efforts include trying to block the entry of calcium ions into muscle cells.[80]
Exon-skipping
[edit]Antisense oligonucleotides (oligos), structural analogs of DNA, are the basis of a potential treatment for 10% of people with Duchenne muscular dystrophy.[81] The compounds allow faulty parts of the dystrophin gene to be skipped when it is transcribed to RNA for protein production, permitting a still-truncated but more functional version of the protein to be produced.[82] It is also known as nonsense suppression therapy.[83]
Two kinds of antisense oligos, 2'-O-methyl phosphorothioate oligos (like Drisapersen) and Morpholino oligos (like eteplirsen), have tentative evidence of benefit and are being studied.[84] Eteplirsen is targeted to skip exon 51.[84] "As an example, skipping exon 51 restores the reading frame of ~ 15% of all the boys with deletions. It has been suggested that by having 10 AONs to skip 10 different exons it would be possible to deal with more than 70% of all DMD boys with deletions."[81] This represents about 1.5% of cases.[81]

People with Becker's muscular dystrophy, which is milder than DMD, have a form of dystrophin which is functional even though it is shorter than normal dystrophin.[85] In 1990 England et al. noticed that a patient with mild Becker muscular dystrophy was lacking 46% of his coding region for dystrophin.[85] This functional, yet truncated, form of dystrophin gave rise to the notion that shorter dystrophin can still be therapeutically beneficial. Concurrently, Kole et al. had modified splicing by targeting pre-mRNA with antisense oligonucleotides (AONs).[86] Kole demonstrated success using splice-targeted AONs to correct missplicing in cells removed from beta-thalassemia patients[87][88] Wilton's group tested exon skipping for muscular dystrophy.[89][90]
Gene therapy
[edit]Researchers are working on a gene editing method to correct a mutation that leads to Duchenne muscular dystrophy (DMD).[91] Researchers used a technique called CRISPR/Cas9-mediated genome editing, which can precisely remove a mutation in the dystrophin gene in DNA, allowing the body's DNA repair mechanisms to replace it with a normal copy of the gene.[92][93]
Genome editing through the CRISPR/Cas9 system is not currently feasible in humans. However, it may be possible, through advancements in technology, to use this technique to develop therapies for DMD in the future.[94][95] In 2007, researchers did the world's first clinical (viral-mediated) gene therapy trial for Duchenne MD.[96]
Biostrophin is a delivery vector for gene therapy in the treatment of Duchenne muscular dystrophy and Becker muscular dystrophy.[97]
Future developments
[edit]Several medications designed to address the root cause are under development, including gene therapy and antisense drugs.[3] Other medications used include corticosteroids to slow muscle degeneration.[2] Physical therapy, orthopedic braces, and corrective surgery may help with some symptoms[2] while assisted ventilation may be required in those with weakness of breathing muscles.[3] Outcomes depend on the specific type of disorder.[98][3]
References
[edit]- ^ "Duchenne". Merriam-Webster.com Dictionary. Merriam-Webster.
- ^ a b c d e f g h i j "NINDS Muscular Dystrophy Information Page". National Institute of Neurological Disorders and Stroke (NINDS). 4 March 2016. Archived from the original on 30 July 2016. Retrieved 12 September 2016.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain.
- ^ a b c d e f g h i j k l m n o p q r s t u v w x y z aa "Muscular Dystrophy: Hope Through Research". National Institute of Neurological Disorders and Stroke (NINDS). 4 March 2016. Archived from the original on 30 September 2016. Retrieved 12 September 2016.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain.
- ^ "Muscular Dystrophy". National Institute of Neurological Disorders and Stroke (NINDS). 30 October 2023. Archived from the original on 31 March 2024. Retrieved 31 March 2024.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain.
- ^ a b c Landfeldt E, Thompson R, Sejersen T, McMillan HJ, Kirschner J, Lochmüller H (2020). "Life expectancy at birth in Duchenne muscular dystrophy: a systematic review and meta-analysis". European Journal of Epidemiology. 35 (7): 643–653. doi:10.1007/s10654-020-00613-8. ISSN 1573-7284. PMC 7387367. PMID 32107739.
- ^ a b c Nozoe KT, Akamine RT, Mazzotti DR, Polesel DN, Grossklauss LF, Tufik S, et al. (2016). "Phenotypic contrasts of Duchenne Muscular Dystrophy in women: Two case reports". Sleep Science. 9 (3): 129–133. doi:10.1016/j.slsci.2016.07.004. PMC 5241604. PMID 28123647.
- ^ "Muscular Dystrophy: Hope Through Research". National Institute of Neurological Disorders and Stroke (NINDS). September 2013. Archived from the original on 31 March 2024. Retrieved 31 March 2024.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain.
- ^ https://catalog.ninds.nih.gov/sites/default/files/publications/muscular-dystrophy-hope-through-research.pdf Archived 31 March 2024 at the Wayback Machine
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain.
- ^ Crisafulli S, Sultana J, Fontana A, Salvo F, Messina S, Trifirò G (June 2020). "Global epidemiology of Duchenne muscular dystrophy: an updated systematic review and meta-analysis". Orphanet Journal of Rare Diseases. 15 (1): 141. doi:10.1186/s13023-020-01430-8. PMC 7275323. PMID 32503598.
- ^ "Duchenne Muscular Dystrophy (DMD)". Muscular Dystrophy Association. 17 November 2017. Archived from the original on 15 November 2022. Retrieved 15 November 2022.
- ^ a b Broomfield J, Hill M, Guglieri M, Crowther M, Abrams K (7 December 2021). "Life Expectancy in Duchenne Muscular Dystrophy: Reproduced Individual Patient Data Meta-analysis". Neurology. 97 (23): e2304–e2314. doi:10.1212/WNL.0000000000012910. ISSN 0028-3878. PMC 8665435. PMID 34645707.
- ^ a b c d e "Duchenne muscular dystrophy". Genetic and Rare Diseases (GARD) Information Center. Archived from the original on 23 November 2016. Retrieved 24 January 2021.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain.
- ^ Angelini C, Tasca E (December 2012). "Fatigue in muscular dystrophies". Neuromuscular Disorders. 22 (Suppl 3): S214–S220. doi:10.1016/j.nmd.2012.10.010. PMC 3526799. PMID 23182642.
- ^ a b Rowland LP (1985). "Clinical Perspective: Phenotypic Expression In Muscular Dystrophy". In Strohman C, Wolf S (eds.). Gene Expression in Muscle. Advances in Experimental Medicine and Biology. Plenum Press. pp. 3–5. ISBN 978-1-4684-4907-5. Archived from the original on 29 September 2020. Retrieved 7 August 2019.
- ^ a b c d e f Darras BT, Urion DK, Ghosh PS (2018). "Dystrophinopathies". GeneReviews. Seattle (WA): University of Washington. PMID 20301298.
- ^ Emery AE, Muntoni F, Quinlivan R (2015). Duchenne Muscular Dystrophy (Fourth ed.). OUP Oxford. ISBN 978-0-19968148-8. Archived from the original on 31 March 2024. Retrieved 27 May 2020.
- ^ a b "Muscular dystrophy - Symptoms and causes". Mayo Clinic. Archived from the original on 6 February 2015. Retrieved 6 February 2015.
- ^ a b c d MedlinePlus Encyclopedia: Duchenne muscular dystrophy
- ^ Sutherland DH, Olshen R, Cooper L, Wyatt M, Leach J, Mubarak S, et al. (February 1981). "The pathomechanics of gait in Duchenne muscular dystrophy". Developmental Medicine and Child Neurology. 23 (1): 3–22. doi:10.1111/j.1469-8749.1981.tb08442.x. PMID 7202868. S2CID 895379.
- ^ Baptista CR, Costa AA, Pizzato TM, Souza FB, Mattiello-Sverzut AC (2014). "Postural alignment in children with Duchenne muscular dystrophy and its relationship with balance". Brazilian Journal of Physical Therapy. 18 (2): 119–126. doi:10.1590/s1413-35552012005000152. PMC 4183248. PMID 24838810.
- ^ Doorenweerd N, Mahfouz A, van Putten M, Kaliyaperumal R, T' Hoen PA, Hendriksen JG, et al. (October 2017). "Timing and localization of human dystrophin isoform expression provide insights into the cognitive phenotype of Duchenne muscular dystrophy". Scientific Reports. 7 (1): 12575. Bibcode:2017NatSR...712575D. doi:10.1038/s41598-017-12981-5. PMC 5626779. PMID 28974727.
- ^ Online Mendelian Inheritance in Man (OMIM): Muscular Dystrophy, Duchenne Type; DMD - 310200
- ^ Vera CD, Zhang A, Pang PD, Wu JC (2022). "Treating Duchenne Muscular Dystrophy: The Promise of Stem Cells, Artificial Intelligence, and Multi-Omics". Frontiers in Cardiovascular Medicine. 9: 851491. doi:10.3389/fcvm.2022.851491. PMC 8960141. PMID 35360042.
- ^ "Duchenne Muscular Dystrophy: Pathophysiological Implications of Mitochondrial Calcium Signaling and ROS Production". 2 May 2012. Archived from the original on 2 May 2012. Retrieved 29 June 2014.
- ^ Wahl M (21 October 2016). "Quest - Article - But Girls Don't Get Duchenne, or Do They? - A Quest Article". Muscular Dystrophy Association. Archived from the original on 12 April 2019. Retrieved 6 July 2019.
- ^ Wucherpfennig J (6 October 2016). "If a man has Duchenne muscular dystrophy, what are the chances his children will have DMD?". The Tech Interactive. Ask a Geneticist. Retrieved 5 August 2024.
- ^ Nico B, Ribatti D (January 2012). "Morphofunctional aspects of the blood–brain barrier". Current Drug Metabolism. 13 (1): 50–60. doi:10.2174/138920012798356970. PMID 22292807.
- ^ "University of Utah Muscular Dystrophy". Genome.utah.edu. 28 November 2009. Archived from the original on 14 September 2003. Retrieved 16 February 2013.
- ^ a b Bushby K, Finkel R, Birnkrant DJ, Case LE, Clemens PR, Cripe L, et al. (January 2010). "Diagnosis and management of Duchenne muscular dystrophy, part 1: diagnosis, and pharmacological and psychosocial management". The Lancet. Neurology. 9 (1): 77–93. CiteSeerX 10.1.1.176.4466. doi:10.1016/s1474-4422(09)70271-6. PMID 19945913. S2CID 328499.
- ^ Nicholson LV, Johnson MA, Bushby KM, Gardner-Medwin D, Curtis A, Ginjaar IB, et al. (September 1993). "Integrated study of 100 patients with Xp21 linked muscular dystrophy using clinical, genetic, immunochemical, and histopathological data. Part 2. Correlations within individual patients". Journal of Medical Genetics. 30 (9): 737–744. doi:10.1136/jmg.30.9.737. PMC 1016530. PMID 8411068.
- ^ Muntoni F (August 2001). "Is a muscle biopsy in Duchenne dystrophy really necessary?". Neurology. 57 (4): 574–575. doi:10.1212/wnl.57.4.574. PMID 11524463. S2CID 13474827.
- ^ Flanigan KM, von Niederhausern A, Dunn DM, Alder J, Mendell JR, Weiss RB (April 2003). "Rapid direct sequence analysis of the dystrophin gene". American Journal of Human Genetics. 72 (4): 931–939. doi:10.1086/374176. PMC 1180355. PMID 12632325.
- ^ Beksac MS, Tanacan A, Aydin Hakli D, Orgul G, Soyak B, Balci Hayta B, et al. (30 July 2018). "Gestational Outcomes of Pregnant Women Who Have Had Invasive Prenatal Testing for the Prenatal Diagnosis of Duchenne Muscular Dystrophy". Journal of Pregnancy. 2018: 9718316. doi:10.1155/2018/9718316. PMC 6091284. PMID 30151283.
- ^ Devaney SA, Palomaki GE, Scott JA, Bianchi DW (August 2011). "Noninvasive fetal sex determination using cell-free fetal DNA: a systematic review and meta-analysis". JAMA. 306 (6): 627–636. doi:10.1001/jama.2011.1114. PMC 4526182. PMID 21828326.
- ^ "Duchenne Muscular Dystrophy Statement". U.S. Food and Drug Administration (FDA). 31 October 2014. Archived from the original on 2 November 2014.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain.
- ^ Dany A, Barbe C, Rapin A, Réveillère C, Hardouin JB, Morrone I, et al. (November 2015). "Construction of a Quality of Life Questionnaire for slowly progressive neuromuscular disease". Quality of Life Research. 24 (11): 2615–2623. doi:10.1007/s11136-015-1013-8. PMID 26141500. S2CID 25834947.
- ^ Falzarano MS, Scotton C, Passarelli C, Ferlini A (October 2015). "Duchenne Muscular Dystrophy: From Diagnosis to Therapy". Molecules. 20 (10): 18168–18184. doi:10.3390/molecules201018168. PMC 6332113. PMID 26457695.
- ^ Matthews E, Brassington R, Kuntzer T, Jichi F, Manzur AY (May 2016). "Corticosteroids for the treatment of Duchenne muscular dystrophy". The Cochrane Database of Systematic Reviews. 5 (5): CD003725. doi:10.1002/14651858.CD003725.pub4. PMC 8580515. PMID 27149418.
- ^ a b "Duchenne Muscular Dystrophy". Physiopedia. Archived from the original on 10 October 2022. Retrieved 10 October 2022.
- ^ Pedlow K, McDonough S, Lennon S, Kerr C, Bradbury I (October 2019). "Assisted standing for Duchenne muscular dystrophy". The Cochrane Database of Systematic Reviews. 10 (10): CD011550. doi:10.1002/14651858.CD011550.pub2. PMC 6790222. PMID 31606891.
- ^ Verhaert D, Richards K, Rafael-Fortney JA, Raman SV (January 2011). "Cardiac involvement in patients with muscular dystrophies: magnetic resonance imaging phenotype and genotypic considerations". Circulation: Cardiovascular Imaging. 4 (1): 67–76. doi:10.1161/CIRCIMAGING.110.960740. PMC 3057042. PMID 21245364.
- ^ "Railroading at the FDA". Nature Biotechnology. 34 (11): 1078. November 2016. doi:10.1038/nbt.3733. PMID 27824847.
- ^ "FDA grants accelerated approval to first drug for Duchenne muscular dystrophy" (Press release). U.S. Food and Drug Administration (FDA). 19 September 2016. Archived from the original on 2 August 2019. Retrieved 8 July 2019.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain.
- ^ "CHMP Advises Against Approval for Eteplirsen in DMD". Medscape. Archived from the original on 9 July 2019. Retrieved 9 July 2019.
- ^ "Exondys". European Medicines Agency. 17 September 2018. Archived from the original on 26 November 2020. Retrieved 3 December 2022.
- ^ "Translarna EPAR". European Medicines Agency (EMA). Archived from the original on 29 October 2020. Retrieved 14 August 2020.
- ^ "Translarna - Summary of Product Characteristics (SmPC)". (emc). 24 April 2017. Archived from the original on 15 July 2017. Retrieved 18 June 2017.
- ^ "FDA grants accelerated approval to first targeted treatment for rare Duchenne muscular dystrophy mutation" (Press release). U.S. Food and Drug Administration (FDA). 12 December 2019. Archived from the original on 13 December 2019. Retrieved 12 December 2019.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain.
- ^ "Drug Approval Package: Vyondys 53 (golodirsen)". U.S. Food and Drug Administration (FDA). 21 January 2020. Archived from the original on 2 March 2020. Retrieved 22 January 2020.
- ^ a b c "FDA Approves Targeted Treatment for Rare Duchenne Muscular Dystrophy Mutation" (Press release). U.S. Food and Drug Administration (FDA). 12 August 2020. Archived from the original on 20 August 2020. Retrieved 12 August 2020.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain.
- ^ Yokota T, Lu QL, Partridge T, Kobayashi M, Nakamura A, Takeda S, et al. (June 2009). "Efficacy of systemic morpholino exon-skipping in Duchenne dystrophy dogs". Annals of Neurology. 65 (6): 667–676. doi:10.1002/ana.21627. ISSN 1531-8249. PMC 5951302. PMID 19288467.
- ^ a b "FDA Approves Targeted Treatment for Rare Duchenne Muscular Dystrophy Mutation" (Press release). U.S. Food and Drug Administration (FDA). 25 February 2021. Archived from the original on 3 August 2021. Retrieved 25 February 2021.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain.
- ^ Birnkrant DJ, Bushby K, Bann CM, Apkon SD, Blackwell A, Brumbaugh D, et al. (March 2018). "Diagnosis and management of Duchenne muscular dystrophy, part 1: diagnosis, and neuromuscular, rehabilitation, endocrine, and gastrointestinal and nutritional management". The Lancet. Neurology. 17 (3): 251–267. doi:10.1016/S1474-4422(18)30024-3. PMC 5869704. PMID 29395989.
- ^ Birnkrant DJ, Bushby K, Bann CM, Alman BA, Apkon SD, Blackwell A, et al. (April 2018). "Diagnosis and management of Duchenne muscular dystrophy, part 2: respiratory, cardiac, bone health, and orthopaedic management". The Lancet. Neurology. 17 (4): 347–361. doi:10.1016/S1474-4422(18)30025-5. PMC 5889091. PMID 29395990.
- ^ "FDA Approves First Gene Therapy for Treatment of Certain Patients with Duchenne Muscular Dystrophy" (Press release). U.S. Food and Drug Administration (FDA). 22 June 2023. Archived from the original on 29 November 2023. Retrieved 22 June 2023.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain.
- ^ "Sarepta Therapeutics Announces FDA Approval of Elevidys, the First Gene Therapy to Treat Duchenne Muscular Dystrophy" (Press release). Sarepta Therapeutics. 22 June 2023. Archived from the original on 23 June 2023. Retrieved 22 June 2023 – via Business Wire.
- ^ "FDA Approves Nonsteroidal Treatment for Duchenne Muscular Dystrophy". U.S. Food and Drug Administration (FDA) (Press release). 21 March 2024. Archived from the original on 23 March 2024. Retrieved 23 March 2024.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain.
- ^ Lisak RP, Truong DD, Carroll W, Bhidayasiri R (2011). International Neurology. Wiley. p. 222. ISBN 978-1-4443-1701-5.
- ^ "Duchenne muscular dystrophy (DMD) | Muscular Dystrophy Campaign". Muscular-dystrophy.org. Archived from the original on 21 January 2013. Retrieved 16 February 2013.
- ^ Medvescek C (31 October 2005). "Quest - Article - Despite the Challenge, People Love Their Live-Ins". Muscular Dystrophy Association. Retrieved 2 October 2024.
- ^ "Rotary to offer Russian visit; North shuffle to be Aug. 26". The Sun Chronicle. 24 August 2008. Retrieved 2 October 2024.
- ^ Kieny P, Chollet S, Delalande P, Le Fort M, Magot A, Pereon Y, et al. (September 2013). "Evolution of life expectancy of patients with Duchenne muscular dystrophy at AFM Yolaine de Kepper centre between 1981 and 2011". Annals of Physical and Rehabilitation Medicine. 56 (6): 443–454. doi:10.1016/j.rehab.2013.06.002. PMID 23876223.
- ^ Krajina A, Podrabský P, Steinhart L, Endrys J, Coufal L (22 November 2012). "[Personal experimental experience with the administration of liquid obliterative agents using percutaneous intra-arterial balloon catheters with a controlled leak]". Sbornik Vedeckych Praci Lekarske Fakulty Karlovy Univerzity V Hradci Kralove. Supplementum. 30 (2): 201–211. doi:10.1186/1750-1172-7-S2-A8. PMC 3504593. PMID 3504593.
- ^ Marques MJ, Ferretti R, Vomero VU, Minatel E, Neto HS (March 2007). "Intrinsic laryngeal muscles are spared from myonecrosis in the mdx mouse model of Duchenne muscular dystrophy". Muscle & Nerve. 35 (3): 349–353. doi:10.1002/mus.20697. PMID 17143878. S2CID 41968787.
- ^ Ferretti R, Marques MJ, Khurana TS, Santo Neto H (June 2015). "Expression of calcium-buffering proteins in rat intrinsic laryngeal muscles". Physiological Reports. 3 (6): e12409. doi:10.14814/phy2.12409. PMC 4510619. PMID 26109185.
- ^ White Z, Hakim CH, Theret M, Yang NN, Rossi F, Cox D, et al. (July 2020). "High prevalence of plasma lipid abnormalities in human and canine Duchenne and Becker muscular dystrophies depicts a new type of primary genetic dyslipidemia". Journal of Clinical Lipidology. 14 (4): 459–469.e0. doi:10.1016/j.jacl.2020.05.098. PMC 7492428. PMID 32593511. S2CID 219741257.
- ^ "Population-Based Prevalence of Duchenne and Becker Muscular Dystrophies in the United States". U.S. Centers for Disease Control and Prevention (CDC). 5 January 2018. Archived from the original on 18 November 2018. Retrieved 18 November 2018.
- ^ Romitti PA, Zhu Y, Puzhankara S, James KA, Nabukera SK, Zamba GK, et al. (March 2015). "Prevalence of Duchenne and Becker muscular dystrophies in the United States". Pediatrics. 135 (3): 513–21. doi:10.1542/peds.2014-2044. PMC 4477633. PMID 25687144.
- ^ Politano L. "Cardiomiologia e Genetica Medica" [Cardiomyology and Medical Genetics] (in Italian). Seconda Università degli Studi di Napoli. Archived from the original on 4 July 2015. Retrieved 24 August 2015.
- ^ De Rosa G (October 2005). "Da Conte a Duchenne" [By Conte in Duchenne]. DM (in Italian). Unione Italiana Lotta alla Distrofia Muscolare. Archived from the original on 4 March 2016. Retrieved 24 August 2015.
- ^ Nigro G (December 2010). "One-hundred-seventy-five years of Neapolitan contributions to the fight against the muscular diseases". Acta Myologica. 29 (3): 369–391. PMC 3146338. PMID 21574522.
- ^ "Duchenne muscular dystrophy". Medterms.com. 27 April 2011. Archived from the original on 6 August 2012. Retrieved 16 February 2013.
- ^ Duchenne de Boulogne at Who Named It?
- ^ Susanna Kim (21 October 2015). "What You Didn't Know About the Ferrari Family". ABC News. Archived from the original on 31 August 2023. Retrieved 31 August 2023.
- ^ The GearShifters Team (13 September 2022). "How Did Dino Ferrari Die?". GearShifters. Archived from the original on 31 August 2023. Retrieved 31 August 2023.
- ^ McFadden C, Johnson E, Effron L (22 November 2012). "Darius Weems' Next Chapter: Rap Star With Duchenne Muscular Dystrophy Tries Clinical Trial". ABC News. Archived from the original on 5 August 2016. Retrieved 29 June 2016.
- ^ Eric Johnson (10 October 2016). "Disability Rights Activist Darius Weems Loses Battle with Duchenne Muscular Dystrophy". ABC News. Archived from the original on 31 August 2023. Retrieved 31 August 2023.
- ^ Berkshire G (23 January 2016). "Sundance Film Review: 'The Fundamentals of Caring'". Variety. Archived from the original on 21 October 2021. Retrieved 21 October 2021.
- ^ Guiraud S, Davies KE (June 2017). "Pharmacological advances for treatment in Duchenne muscular dystrophy". Current Opinion in Pharmacology. 34: 36–48. doi:10.1016/j.coph.2017.04.002. PMID 28486179.
- ^ Allen DG, Gervasio OL, Yeung EW, Whitehead NP (February 2010). "Calcium and the damage pathways in muscular dystrophy". Canadian Journal of Physiology and Pharmacology. 88 (2): 83–91. doi:10.1139/Y09-058. PMID 20237582.
- ^ a b c Scoto M, Finkel R, Mercuri E, Muntoni F (August 2018). "Genetic therapies for inherited neuromuscular disorders". The Lancet. Child & Adolescent Health. 2 (8): 600–609. doi:10.1016/S2352-4642(18)30140-8. PMID 30119719. S2CID 52032568. Archived from the original on 17 August 2021. Retrieved 16 November 2022.
- ^ Dunckley MG, Manoharan M, Villiet P, Eperon IC, Dickson G (July 1998). "Modification of splicing in the dystrophin gene in cultured Mdx muscle cells by antisense oligoribonucleotides". Human Molecular Genetics. 7 (7): 1083–1090. doi:10.1093/hmg/7.7.1083. PMID 9618164.
- ^ Finkel RS (September 2010). "Read-through strategies for suppression of nonsense mutations in Duchenne/ Becker muscular dystrophy: aminoglycosides and ataluren (PTC124)". Journal of Child Neurology. 25 (9): 1158–1164. doi:10.1177/0883073810371129. PMC 3674569. PMID 20519671.
- ^ a b "FDA grants accelerated approval to first drug for Duchenne muscular dystrophy" (Press release). U.S. Food and Drug Administration (FDA). 19 September 2016. Archived from the original on 11 December 2016. Retrieved 12 December 2016.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain.
- ^ a b England SB, Nicholson LV, Johnson MA, Forrest SM, Love DR, Zubrzycka-Gaarn EE, et al. (January 1990). "Very mild muscular dystrophy associated with the deletion of 46% of dystrophin". Nature. 343 (6254): 180–182. Bibcode:1990Natur.343..180E. doi:10.1038/343180a0. PMID 2404210. S2CID 4349360.
- ^ Dominski Z, Kole R (September 1993). "Restoration of correct splicing in thalassemic pre-mRNA by antisense oligonucleotides". Proceedings of the National Academy of Sciences of the United States of America. 90 (18): 8673–8677. Bibcode:1993PNAS...90.8673D. doi:10.1073/pnas.90.18.8673. PMC 47420. PMID 8378346.
- ^ Lacerra G, Sierakowska H, Carestia C, Fucharoen S, Summerton J, Weller D, et al. (August 2000). "Restoration of hemoglobin A synthesis in erythroid cells from peripheral blood of thalassemic patients". Proceedings of the National Academy of Sciences of the United States of America. 97 (17): 9591–9596. Bibcode:2000PNAS...97.9591L. doi:10.1073/pnas.97.17.9591. PMC 16909. PMID 10944225.
- ^ Suwanmanee T, Sierakowska H, Lacerra G, Svasti S, Kirby S, Walsh CE, et al. (September 2002). "Restoration of human beta-globin gene expression in murine and human IVS2-654 thalassemic erythroid cells by free uptake of antisense oligonucleotides". Molecular Pharmacology. 62 (3): 545–553. doi:10.1124/mol.62.3.545. PMID 12181431.
- ^ Wilton SD, Lloyd F, Carville K, Fletcher S, Honeyman K, Agrawal S, et al. (July 1999). "Specific removal of the nonsense mutation from the mdx dystrophin mRNA using antisense oligonucleotides". Neuromuscular Disorders. 9 (5): 330–338. doi:10.1016/S0960-8966(99)00010-3. PMID 10407856. S2CID 20678312.
- ^ Wilton SD, Fall AM, Harding PL, McClorey G, Coleman C, Fletcher S (July 2007). "Antisense oligonucleotide-induced exon skipping across the human dystrophin gene transcript". Molecular Therapy. 15 (7): 1288–1296. doi:10.1038/sj.mt.6300095. PMID 17285139.
- ^ Long C, Li H, Tiburcy M, Rodriguez-Caycedo C, Kyrychenko V, Zhou H, et al. (January 2018). "Correction of diverse muscular dystrophy mutations in human engineered heart muscle by single-site genome editing". Science Advances. 4 (1): eaap9004. Bibcode:2018SciA....4.9004L. doi:10.1126/sciadv.aap9004. PMC 5796795. PMID 29404407.
- ^ Cohen J (30 August 2018). "Gene editing of dogs offers hope for treating human muscular dystrophy". Science. doi:10.1126/science.aav2676. S2CID 92204241.
- ^ Patmanathan SN, Gnanasegaran N, Lim MN, Husaini R, Fakiruddin KS, Zakaria Z (2018). "CRISPR/Cas9 in Stem Cell Research: Current Application and Future Perspective". Current Stem Cell Research & Therapy. 13 (8): 632–644. doi:10.2174/1574888X13666180613081443. PMID 29895256. S2CID 48357156.
- ^ Long C, McAnally JR, Shelton JM, Mireault AA, Bassel-Duby R, Olson EN (September 2014). "Prevention of muscular dystrophy in mice by CRISPR/Cas9-mediated editing of germline DNA". Science. 345 (6201): 1184–1188. Bibcode:2014Sci...345.1184L. doi:10.1126/science.1254445. PMC 4398027. PMID 25123483.
- ^ Wade N (31 December 2015). "Gene Editing Offers Hope for Treating Duchenne Muscular Dystrophy, Studies Find". The New York Times. Archived from the original on 2 January 2016. Retrieved 1 January 2016.
- ^ Rodino-Klapac LR, Chicoine LG, Kaspar BK, Mendell JR (September 2007). "Gene therapy for duchenne muscular dystrophy: expectations and challenges". Archives of Neurology. 64 (9): 1236–1241. doi:10.1001/archneur.64.9.1236. PMID 17846262.
- ^ Khurdayan VK, Bozzo J, Prous JR (October 2005). "Chronicles in drug discovery". Drug News & Perspectives. 18 (8): 517–522. doi:10.1358/dnp.2005.18.8.953409. PMID 16391721.
- ^ "NINDS Muscular Dystrophy Information Page". NINDS. 4 March 2016. Archived from the original on 30 July 2016. Retrieved 12 September 2016.
